Daniel R. Jensen and Dr. James P. Porter, Department of Physiology and Developmental Biology
The “Spontaneously Hypertensive Rat” strain (SHR) was bred to be innately hypertensive. This hypertension arises in part from over-activity of the brain Renin-Angiotensin system.1 Interestingly, the mean body weight of SHR is significantly reduced compared with the normotensive Wistar-Kyoto strain from which it originates. There are indications that high levels of exogenous Angiotensin II (ANG II) introduced in the brains of normotensive rats inhibit weight gain, and in some cases promote weight loss and/or wasting.2 The mechanism of this effect is not clearly understood, though some studies have shown that high levels of exogenous ANG II can induce anorexia or increase thermogenic activity in the brown adipose tissue (BAT.)3 SHR presents an ideal model for the study of this phenomenon because the elevated brain ANG II levels are endogenous, whereas previous studies have focused on exogenous, artificially high levels of ANG II, introduced intracerebroventricularly (ICV) into normotensive rats, generally Sprague Dawley. To our knowledge, the role of endogenous brain ANG II in control of body weight has never been investigated.
The Purpose of this study was to assess the role of brain ANG II in inhibiting growth. We hypothesized that SHR would grow beyond its normal size if the action of ANG II in the brain were blocked by ICV administration of Losartan, an ANG II receptor antagonist. We further predicted that weight gains would be a result of increased eating, and also decreased energy expenditure from the BAT.
All rats received either Losartan (32 ng/minute) or saline ICV via a minipump for two weeks. During this time, weight, food consumption and drinking were measured daily. All rats were males. 5 SHR rats received ICV Losartan and were allowed to eat ad libitum. 5 SHR rats received ICV saline (as a negative control,) and also were allowed to eat ad libitum. 5 SHR rats received ICV Losartan, but were also pair fed with the SHR saline group to identify the presence of factors other than increased food consumption. Since the saline group was expected to eat less than the first Losartan group, any weight gain in the pair fed group would indicate that other factors, such as BAT energy expenditure, had been altered. Finally, 5 Wistar-Kyoto rats (WKY) received ICV saline, and were allowed to eat ad libitum for purposes of comparison. We hypothesized that the Losartan SHR group would be similar to the saline WKY group in food consumption and weight gain.
At the end of the two-week study, blood pressure was measured via catheterization of the femoral artery to determine the possibility of changes in blood pressure as a confounding factor. No significant difference was detected. Brain sections were prepared for In-Situ Receptor Autoradiography4 using radioactive ANG II to bind to the AT1a receptor in the paraventricular nucleus of the hypothalamus. This was intended to verify that Losartan administration had been successful. The Losartan treated rats should show reduced binding, since the Losartan acts as an ANG II receptor antagonist, while the other groups should exhibit normal levels of binding. In order to test for changes in energy expenditure in the BAT, total BAT RNA was isolated and reverse transcribed. The reverse transcribed DNA was then run through PCR with primers for the Uncoupling Protein Gene (UCP). (Uncoupling protein is largely responsible for thermogenic activity in the BAT.) Upon electrophoresis, optical density of the UCP band was determined and compared with the 18s rRNA band in order to compare UCP transcription levels.5 A relative decrease UCP expression in the treated SHR groups would indicate reduced energy expenditure in the BAT.
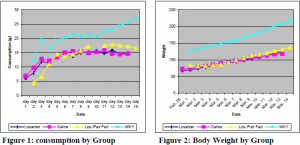
Our results were surprising, however. Contrary to expectations, the Losartan treated groups exhibited no significant change in food or water consumption, and no significant weight gain beyond that exhibited in the saline group (see figures below). We also observed no marked effect on blood pressure or heart rate (p=.138 and .226, respectively). We attempted to compare energy expenditure in the BAT of the different groups, but obtained poor results in the isolation of UCP mRNA. Since there was no significant difference in weight gain or consumption between the different SHR groups, however, we can infer that there must also have been no significant difference in thermogenic energy expenditure.
We believe that these data indicate that brain ANG II does not play a significant role in reduced growth of SHR. ICV administration of Losartan showed no demonstrable increase in food consumption or weight gain. These results put in question the possible role of endogenous brain ANG II in mediating any long-term anorexia or thermogenesis. A word of caution is in order, however. In-Situ binding showed a moderate decrease in ANG II binding in the Paraventricular Nucleus of the Hypothalamus in Losartan treated rats, but it could not be shown to be statistically significant (p=.112). It is therefore possible that insufficient Losartan was administered, or that the administration procedure failed. Thus, our data support the nul hypothesis-that brain ANG II does not significantly influence the growth of SHR-but only weakly, since we cannot confirm conclusively that our treatment took effect.