Andrew Barlow, Trevor Lloyd, Mason Poffenbarger, Austin Ricks, Dr. Jeffery Tessem; Nutrition, Dietetics, and Food Science
Introduction
Diabetes’ prevalence is increasing at an alarming rate. Normally, insulin-secreting β-cells in the pancreas regulate proper glucose absorption and storage. Type 1 and Type 2 diabetes are characterized by decreased functional β-cell mass and insulin production (1). Diabetes also results in increased circulating glucose and fatty acid levels, which damage and destroy β-cells over time (2). Our study sheds further light on the palmitate and oleate-induced effects of gradually worsening hyperlipidemia and the mechanisms behind those effects; ultimately, promoting investigation into methods by which existing β-cells could be protected from harmful hyperlipidemia.
Methodology
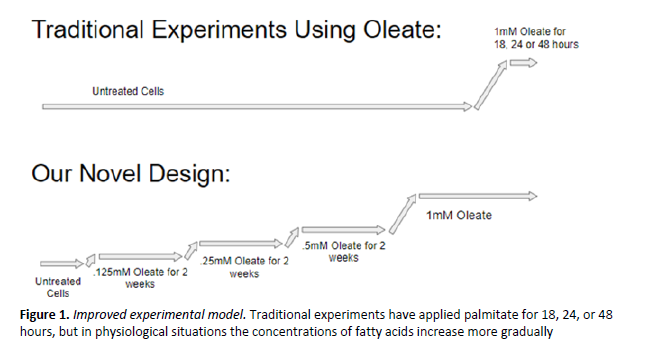
Hyperlipidemia functions as both a cause and a result of T2D, representing a destructive positive feedback loop. Strategies for replacing functional β-cell mass as a treatment for diabetes requires some means of protecting β-cells from continued stress and damage from hyperglycemia and hyperlipidemia. While the short-term effects of hyperlipidemia on functional β-cell mass are well accepted, little is known about how the β-cell adapts to these progressive changes. Most studies have focused on short-term (24-48 hours) incubation in a high concentration of a given FFA, typically palmitate. Physiologically, however, hyperlipidemia is a chronic problem, with a progressive increase in FFA levels. Our study utilizes a novel method of culturing β-cells in progressively increasing concentrations of either the saturated fatty acid palmitate, the most commonly found fatty acid in the human body (3), or the unsaturated fatty acid oleate (see figure 1). Culturing β-cells in fatty acids has allowed us to better elucidate the effects of chronic hyperlipidemia and their mechanisms.
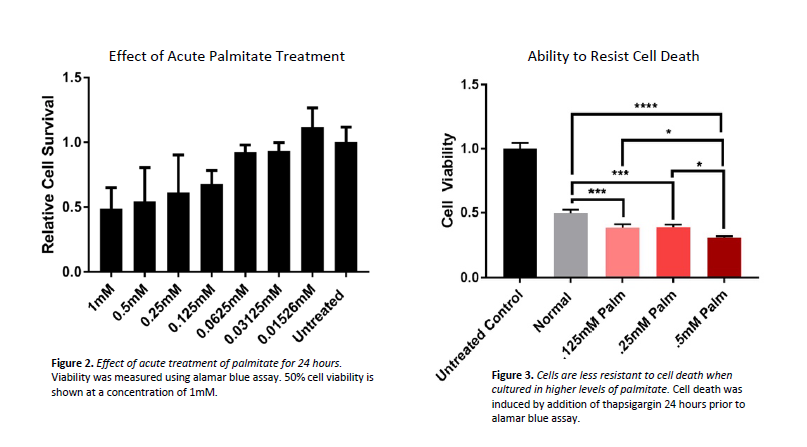
We began by culturing INS-1 cells in 1mM palmitate to see if we could replicate other experiments which consistently observed 50% cell death at said concentration. After confirming our protocol’s effectiveness (see figure 2), we moved on to observe the long-term effects of hyperlipidemia on β- cells by culturing cells in different levels of oleate or palmitate.
Discussion/Results
After performing at least three alamar blue assays to test cell viability on cells cultured in different levels of palmitate, we obtained results consistent with our hypothesis. Cells that were cultured in increasingly higher levels of palmitate and treated with thapsigargin (a drug that induces cell death) were more susceptible to death (See figure 3).
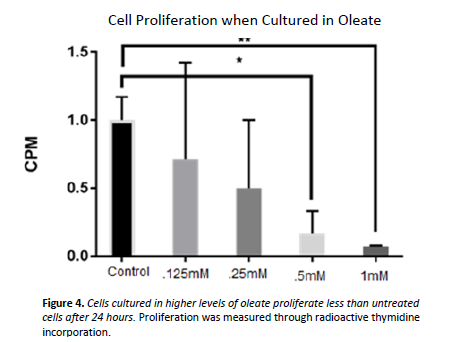
We had trouble gathering consistent data to show the effect of chronic palmitate exposure on proliferation, but we did gather data that showed the effect of acute oleate treatment on proliferation. By using radioactive thymidine incorporation assays, we showed that increasing the concentration of oleate in cell culture media decreases a cell’s ability to proliferate (see figure 4).
Conclusions
We gathered important data that helps us better understand a cell’s ability to resist cell death when cultured in increasingly higher levels of palmitate, but we still need to look into the mechanisms by which this occurs. We will move forward to learn more about how cells exposed to palmitate proliferate and secrete insulin in response to glucose. Additionally, we will perform the same assays on cells chronically exposed to oleate.
Sources
1. Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit 593 and increased beta594 cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52:102-10.
2. Boden, G. and Shulman, G. I. (2002), Free fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and β-cell dysfunction. European Journal of Clinical Investigation, 32: 14–23. doi:10.1046/j.1365-2362.32.s3.3.x.
3. Carta, Gianfranca, Murru, Elisabetta, Banni, Sebastino, and Manca Claudia. Palmitic Acid: Physiological Role, Metabolism and Nutritional Implications. Front Physiol. 2017; 8: 902.