Kayleigh Ingersoll and Faculty Mentor: Dr. Brad Berges, Department of Molecular and Microbiology
Introduction
Human T-lymphotropic virus type-1 (HTLV-1) is a virus that is linked to Adult T-cell leukemia/lymphoma (ATLL), causing cancer in T cells. There are an estimated 10-20 million people worldwide infected with HTLV-1. HTLV-1 is transmitted through contact of bodily fluid and usually occurs through breastfeeding, sexual transmission, and sharing needles. ATLL develops in only about 5% of infected persons after decades of infection. An ATLL diagnosis is grim as there is no cure, and most patients do not respond or only have a limited response to treatments. Current treatments include antiretrovirals or chemotherapy, but there has been little to no research in developing a specific treatment for HTLV-1 induced ATLL other than in clinical trials of terminally ill patients. This project studied the development of cancer from HTLV-1 infection. The purpose of this project was to develop a viable animal model to mirror the infection of HTLV-1 and cancer development of humans in humanized mice.
HTLV-1 infects human CD4+ T-cells and causes out of control proliferation. There is no effective way of studying HTLV-1 infection or ATLL in animal models because of the extended latency period, which is the time from when a person is infected with HTLV-1 to when they develop cancer. Humanized mice develop disease in just weeks rather than decades, making it an exceptional model as it is easy to observe in a short period of time. Normal mouse cells do not have the HTLV-1 viral receptors so the virus cannot infect the cells. This is why we used humanized mice, which are mice transplanted with human immune stem cells, to model the infection in humans and study its effects. The importance of this project is that it could become foundational for the study of HTLV-1 as there is a lack of animal models that faithfully show human disease. This project sought to develop a model to study not only the development of ATLL from HTLV-1, but also to possibly test for treatments in the future.
Methodology
I isolated human stem cells from human umbilical cord blood which were engrafted into immunodeficient pups to create humanized mice. Then the humanized mice were infected with HTLV-1 and observed over a 5-month period. To determine if the virus increased the number of T cells (indicating cancer development), I collected blood samples weekly and ran them through the flow cytometer. Viral levels were measured with quantitative PCR to ascertain the activity of the virus depending on where the viral genome was found and if it was in the RNA or DNA form.
Results
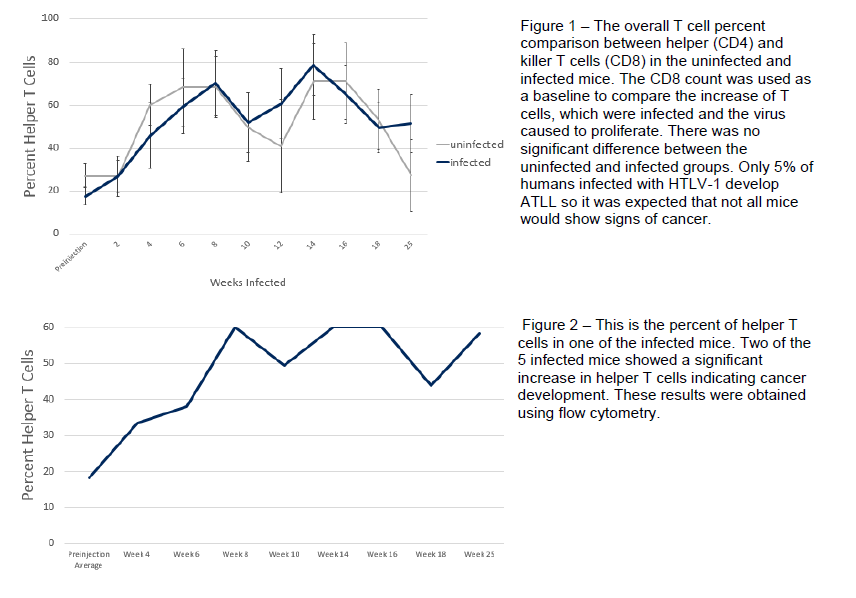
After 5 months, all groups of mice were sacrificed and their immune organs (spleen, thymus and bone marrow) were analyzed for T cell counts. As expected, we observed an increase in the number of T cells in some, but not all, of the experimental mice which
mirrors the 5% of humans infected with HTLV-1 who develop cancer. See figures 1 and 2 below for actual data.
Discussion
This data is promising as it shows that humanized mice can sustain HTLV-1 infection and possibly develop cancer in their T cells just as humans do. Therefore we are duplicating the experiment to verify our initial data and plan to publish the results following the completion of our second experimental trial.
Conclusion
Working closely with Dr. Berges on this project taught me practical skills that I can use in my future career. I learned many different laboratory techniques including how to work with mice, create humanized mice, extract DNA and RNA from blood samples, prepare and run samples in the flow cytometer, and prepare and run samples in the Quantitative PCR machine. I learned critical experimental skills as we had to modify our original plan when a procedure did not show the desired results. I also learned communication techniques as I presented a poster on this project at the Utah Conference for Undergraduate Research, American Society of Microbiology intermountain branch meeting, and the BYU Library Poster Competition. The skills I developed doing this research provided me with the background necessary to apply for and receive an internship through Harvard Medical School’s Immunology Department.