Carrie Draney and Jeffrey Tessem, Nutrition, Dietetics and Food Science
Introduction
Type 1 and type 2 diabetes affects more than 9% of the American population and the incidences of diabetes continue to increase at a startling rate. Both Type 1 and Type 2 diabetes impede β- cell function (insulin secretion) by destroying β-cell mass. Increasing proliferation and function of β-cells could potentially be used as a cure for diabetes. Research has shown that the homeobox β-cell transcription factor Nkx6.1 induces β-cell proliferation. We have found that Nkx6.1 upregulates expression of HDAC1 and this project will allow us to further define the specific role of HDAC1 in increasing β-cell proliferation. We hypothesize that HDAC1 is essential in the β-cell proliferation pathway and could be used to increase insulin secretion and protect against cellular apoptosis.
Methods
In my research INS-1 832-3 cell line was used. Cells were treated with transformed adenoviral vectors for four hours in order to overexpress HDAC1. Untreated β-cells were compared to cells transduced with AdCMV-Bgal and AdCMV-HDAC1. At 96 hours, three separate apoptotic drugs were added in order to induce apoptosis: etoposide, thapsigargin, and campothecin. Cells were counted using a hemocytometer and a 1/10 dilution with PBS was made while counting. For GSIS experiments, untreated β-cells (negative control) were compared to β-cells transduced with AdCMV-GFP (viral control) and AdCMV-HDAC1 (experimental factor). 96 hours after viral transduction, β-cells were assayed for insulin secretion by culturing with low and high glucose to measure GSIS. Insulin was measured by radioimmunoassy, using 125I labeled insulin.
Results
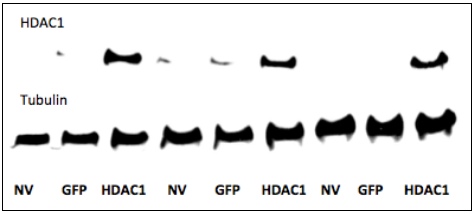
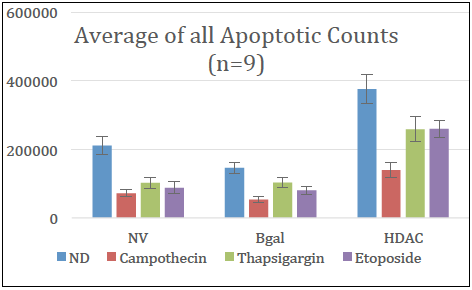
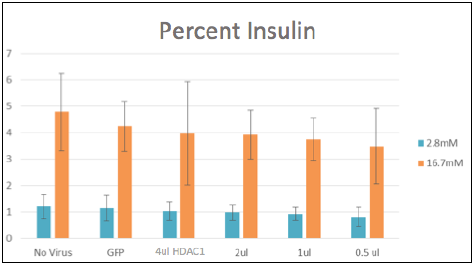
Through western blotting we were able to see proper overexpression of HDAC1 after four hours of viral treatment (Figure 1). After viral transduction and apoptotic drugs were added, cells were counted and the results were analyzed and statistical significance was observed. Data showed overexpression of HDAC1 drove β-cell proliferation when compared to untreated β-cells and AdCMV-Bgal (control and viral control). Data also showed HDAC1 could protect against apoptosis from cells treated with thapsigargin and etoposide (Figure 2). This data suggests HDAC1 has the ability to protect cells from apoptotic stimuli. The inability of HDAC1 to protect against campothecin could be related to its different mode of action. With positive results, the effect of HDAC1 on insulin secretion was examined. Through glucose stimulated insulin secretion, data showed HDAC1 had no negative effect on insulin secretion. Data showed insulin levels were maintained and comparable to untreated cells and AdCMV-GFP (Figure 3).
Discussion & Conclusion
This project has helped further define the role of HDAC1 in the β-cell proliferation pathway. Our results demonstrate HDAC1’s ability to increase β-cell proliferation while maintaining insulin secretion. Maintaining insulin secretion while causing proliferation could indicate the β-cells produced are functioning properly and that overexpression of HDAC1 does not alter the insulin secretion pathway. Furthermore, a major cause of insulin deficiency in diabetes is β-cell apoptosis. As our results demonstrate, HDAC1 has the ability to project cells again apoptosis. This effect would help in the β-cell proliferation pathway to maintain β-cell expansion. This data supports our hypothesis that HDAC1 is essential in the β-cell proliferation pathway. Further study is needed to identify the mechanisms for which HDAC1 induces protection and proliferation. Also conducting these studies in islets would be beneficial to see if similar effects are observed.
Figure 1: Western blot showing HDAC1 expression after INS-‐1 832-‐3 cell line were treated with adenovirus for four hours.
Figure 2: Cells counts for cells treated with NV, Bgal, and HDAC1 and with ND Campothecin, Thapsigargin, or Etoposide. Data shows proliferation of cells and protection against apoptotic stimuli.
Figure 3: GSIS performed on untreated, GFP and HDAC1 treated cells. HDAC1 has no significant effect on percent insulin.