Christopher Stockdale, Joshua Lloyd, and Dr. Robert E. Seegmiller, Physiology and Developmental Biology
Osteoarthritis (OA) is a common disease that causes discomfort and pain due to the degradation of the articular cartilage found on the surface of bones within the body’s joints. A properly functioning joint has a strong network of articular cartilage that can handle the constant strain caused by the use and movement of the joints. Individuals who suffer with OA have a compromised cartilage network that can result in softening of the cartilage, rough joint surfaces, fissures in the cartilage, and eventually direct bone on bone contact within the joint.
Dr. Robert Seegmiller has been characterizing OA and identifying the pathogenesis of the disease for over 25 years. His initial research involved the study of mutant mice which are genetically predisposed to exhibiting early onset OA. These studies have resulted in a hypothesis of a common mechanism of the onset of OA despite the different mutations studied to cause the disease. In collaboration with Dr. Seegmiller we were curious to discover if the mechanism identified in the mutant mice would be similar in mice without a genetic predisposition. This is important to understand because many individuals who do suffer from OA have no apparent genetic predisposition to developing the disease.
In order to provide such a model for our study we called upon Dr. Lin Xu from Harvard University. With the money received through an ORCA grant we flew Dr. Xu to Salt Lake City and invited her to teach us a surgical procedure that could be performed on wildtype mice which would induce OA. The grant also provided us the means to purchase the necessary supplies to perform aseptic surgery on the mice. Dr. Xu spent three days in our lab at Brigham Young University training us how to successfully perform this microsurgery on the right knee of wildtype mice.
From her training we developed a surgical protocol which is now the basis of a new study that we are undertaking in our lab. A summary of the protocol is listed below:
1. Make an incision of the skin on the medial side of patellar ligament using a #15 blade.
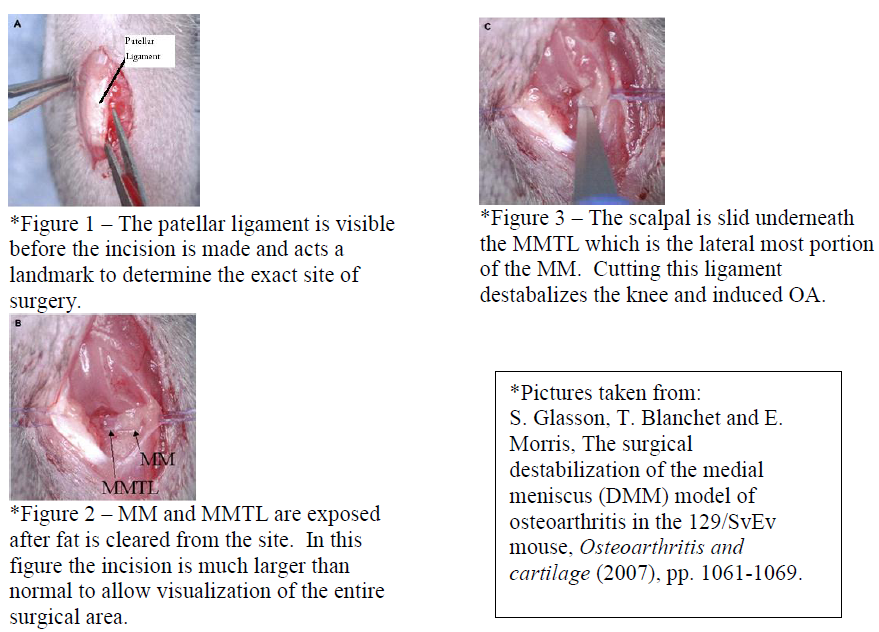
2. Fold back the skin and locate the patellar ligament (Figure 1).
3. Make an incision of the knee capsule on the medial side of the patellar ligament using a #11 blade. The goal is to cause the least amount of trauma as possible by minimizing the size of the incision. The meniscus if found right above the tibia so only cut the capsule toward the bottom of the patellar ligament. After making a very small and superficial incision in the knee capsule, turn the blade upside down and cut upward to increase the length of your incision. Do not cut too deep or too superior as this will cause profuse bleeding and make it very difficult to find the medial meniscus (MM).
4. Push away fat superiorly to expose the MM. The MM should be white and will be the only ligament going medial to lateral (Figure 2).
5. The medial meniscotibial ligament (MMTL) is the lateral most portion of the MM that is visible upon exposing the MM. Carefully slide a #11 blade under the MMTL (Figure 3). When the blade is underneath the MMTL turn it upward at a 45º angle and gently pull upward to incise the MMTL. You can tell when the MMTL is cut because the meniscus becomes loose or limp.
6. Suture capsule back to patellar ligament using a #7-0 coated Vicryl suture. Only one stitch is necessary for closing the capsule.
7. Suture the skin using the same suture. Closing the skin requires 2 stitches.
Initially the surgical procedure was very challenging. The mouse knee is a very small joint to work on and required the use of a dissection microscope to properly perform the surgery. We began practicing the surgery on euthanized mice until we felt confident that we could perform the procedure on live mice without causing excessive trauma. We asked Dr. David Kooyman to oversee our survival surgeries due to his previous experience with operating on mice. To date we have successfully performed 28 surgeries that do exhibit OA. We are looking forward to presenting our findings at an OA conference as well as have a publication on the horizon. In the future we plan on extending our initial aims of the project to include a study of the systemic reaction caused by inducing OA in the right knee. Our hypothesis is that OA will be present in all joints throughout the body despite only having physically altered the right knee.