Trenden Flanigan and Dr. Eric Wilson, Department of Microbiology and Molecular Biology
Abstract
Malaria causes over 1 million deaths every year worldwide. Due to the difficulty in obtaining a precise diagnosis, combined with nonspecific symptoms in early stages (fever, aches, fatigue), many cases are misdiagnosed. Diagnosis methods are generally done through visual examination of peripheral blood smears or rapid diagnostic tests. Due to transient low levels of parasitemia in patients, these diagnostic methods often result in false negatives. By separating the parasitized erythrocytes from the others, the sensitivity of diagnostic tests improves. This was demonstrated by using a novel blood smear technique that introduces centrifugation and isolation into the conventional smear or by using gravitational sedimentation and isolation of whole blood in a capillary tube prior to microscopic analysis. Both of these methods yielded substantial increases in test sensitivity and reduction of false negatives, making diagnosis both easier and more accurate without significantly raising costs to the patient or clinic.
Method
Results were obtained using 205 samples obtained from A Clínica de Saúde de Alto Maé and Hospital Central de Maputo in malaria endemic Maputo, Mozambique. Samples coming into the lab were labeled anonymously and tested in triplicate (one each for the conventional, centrifuged and sedimented methods). Samples were individually read microscopically from the same patient to allow for anonymity as prior status of malaria was unknown.
Analysis
Every year, there are approximately 300-500 million cases of malaria worldwide, leading to the death of between one to three million people.1 The vast majority of these cases occur in Sub-Saharan Africa, such as Mozambique. Diagnostic and treatment problems often arise because these countries are often underdeveloped and lack sufficient funding for expensive modern diagnostic techniques, such as PCR, regardless of their efficacy. Cost is therefore a significant contributing factor to effective treatment of malaria in developing countries.
Currently, the most widespread malarial diagnostic technique is the conventional blood smear. This has been regarded as the “gold standard” of malaria diagnoses. However, due to transient low levels of parasitemia in malaria-positive patients, this diagnostic method often results in false negatives. Therefore, to improve the probability of a true negative, this test should be repeated 3 times at various intervals to ensure no false negatives were recorded.2 This is an expensive and inefficient process that many rural clinics simply cannot afford. By increasing the sensitivity of the original test, the analysis earns confidence without significantly raising costs.
A novel approach to improve the identification of parasitized red blood cells has been developed. Parasitized red blood cells have a different density than other red blood cells. Labs can take advantage of this difference by sedimenting the blood using either gravitational sedimentation or centrifugation. The sedimented concentration of the parasitic red blood cells is therefore increased
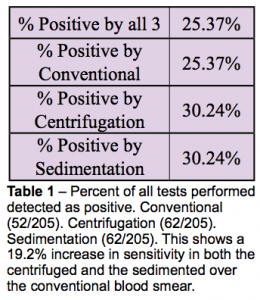
prior to analysis on a blood smear. The centrifuged method is based on research by Bhandari, et al.3 These researchers were able to improve diagnosis from 86% using conventional methods to near 100% with this new technique. Table 1 shows that this
method works in rural clinics as opposed to a university lab. It also shows that gravitational sedimentation for 4 hours yields the
same percent increase in sensitivity as centrifugation. It should be noted that all of the tests that were positive by the conventional blood smear were also positive by the other two methods. However, there were 10 of the 62 total positives that were determined to be negative by the conventional method that both the centrifuged and sedimented methods detected. The results of all centrifuged tests were identical to those of the sedimented tests. This proves that both the sedimented and centrifuged methods are more sensitive than the conventional analysis.
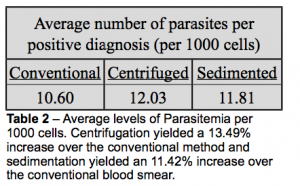
A critical component in determining sensitivity of a test is the average number of parasites per positive test. The parasites were counted and the average values are shown in Table 2. Though the percent increase in test sensitivity between the centrifuged and sedimented tests were identical, the increase in parasitemia was not. The centrifuged method was better at concentrating the
parasites. Regardless of this slight increase in parasitemia, it was not regarded as diagnostically significant as both the sedimented and centrifuged methods had the same increase in sensitivity over the conventional blood smear.
Overall, this research has shown that sedimentation prior to analysis of potentially infected blood markedly increases sensitivity of the test. This means that rural clinics can have confidence in their results and diagnose properly, without raising costs or repeating tests.
All grant funds donated through ORCA were used toward transportation costs and supplies for the project. This research will be presented next spring at the Intermountain branch meeting of the American Society of Microbiology and will be submitted to the Malaria Journal and the Transactions of the Royal Society of Tropical Medicine and Hygiene for publication.
Sources
- Snow, R.W., Guerra, C.A., Noor, A.M., Myint, H.Y., & Hay, S.I. (2005). The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature. 434 (7030), 214–217
- Lalloo, D.G., Shingadia, D., Pasvol, G., Chiodini, P.L., Whitty, C.J., Beeching, N.J., Hill, D.R., Warrell, D.A., & Bannister, B.A. (2007). UK malaria treatment guidelines. British Infection Society. 54 (1), 113.
- Bhandari, P.L., Raghuveer, C.V., Rajeev, A., & Bhandari P.D. (2008). Comparative study of peripheral blood smear and modified centrifuged blood smear in malaria diagnosis. Indian J Pathol Microbiol. 51, 108-112.