David Nolte and Dr. David Kooyman, Physiology and Developmental Biology
Purpose
The purpose of this study is to better understand how osteoarthritis develops.
Background
Osteoarthritis (OA) is the most prevalent form of arthritis, affecting more than 26 million people in the United States1. The condition decreases mobility and causes pain. Furthermore, the spending for medical treatment of osteoarthritis is increasing quickly: Spending doubled from 1994 to 2005. With the increasing age of the U.S. population, prevalence of OA is expected to continue rising1. Thus it is important to find effective treatments to alleviate symptoms and/or prevent osteoarthritis. Recent research has shown that osteoarthritis involves more than just the cartilage of the joint. Synovium and adipose tissue contribute to the breakdown of articular cartilage2. Also, recent research has shown that the biochemistry of articular cartilage plays a significant role in its function and degradation2. The chemical content of extracellular fluid in cartilage is believed to change the function and metabolism of cartilage cells, or chondrocytes3. We hypothesized that one of the metabolic pathways that contributes to osteoarthritis is the unfolded protein response (UPR), a mechanism that protects the endoplasmic reticulum from being damaged by excessive protein buildup. The UPR has been shown to contribute to osteoarthritis in a different mutant mouse model. We are searching for evidence that demonstrates the UPR also contributes to osteoarthritis in the Bardet-Biedl Syndrome mutant mouse model.
Our Research
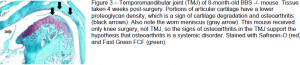
We performed a knee destabilizing surgery on wild type mice and on mice that had a BBS gene knockout. The surgery caused premature development of osteoarthritis. These are the steps we took. Following anesthetization of the mice, we cut the medial meniscal ligament in the right knee of each mouse. This has been shown to destabilize the medial meniscus causing excessive wear of articular cartilage on the surfaces of the tibial plateau and the medial femoral condyle. This wear occurs over time as the mice walk around in their cages. The mice recovered during periods of two and four weeks. After their respective recovery times, the mice were euthanized and tissue samples were taken from the knee, a load-bearing joint, and the temporomandibular joint (TMJ), a non-load-bearing joint. The TMJ serves as a control to ensure that weight load on the knee is not a contributing factor to OA. We then set the samples in paraffin wax, cut them into sections of 10 μm, and stained them for a marker of OA. As the research continues, the tissue samples will be analyzed for signs of osteoarthritis including cartilage thickness, proteoglycan concentration, and chondrocyte density and distribution using the modified Mankin scale. The endoplasmic reticula (ER) in chondrocytes of the cartilage was measured, as larger ER in these cells may indicate the unfolded protein response (UPR) is contributing to osteoarthritis. These data were analyzed and an UPR was detected in BBS mutant mice while not present in wild type controls.
Results and Discussion
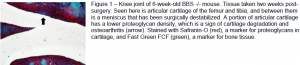
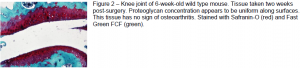
While this project is still in progress, we have some initial results that support our hypothesis that BBS mutant mice exhibit an UPR that may, in part, trigger OA. The mice showed signs of osteoarthritis two and four weeks after surgery. The BBS mouse after four weeks showed an increase in OA (figure 1). The wild type mouse after four weeks showed less OA (figure 2). The TMJ also showed signs of OA, which confirms the premise that OA is a systemic disorder rather than one specific to a joint (figure 3). These
results imply that OA may be triggered by an initial injury/insult resulting in an inflammatory response leading to OA. This is a novel finding. We are preparing a manuscript to document our findings.
Summary and Further Research
Osteoarthritis is a problem for which no effective treatment has been found. With further knowledge of its development and progression, a more effective treatment may be developed. David Kooyman will continue working on this project with his laboratory.
Acknowledgements
This project is funded by the National Institutes of Health (NIH) and the Office of Research and Creative Activities of Brigham Young University. I appreciate David Kooyman for his mentorship and other students who worked on the project, including Danielle Peterson who instructed me on our surgical technique for knee destabilization. Danielle Peterson and I prepared a poster and presented this project at the Life Sciences Student Poster Conference on March 30, 2011.
References
- Gabriel SE, Michaud K. 2009. Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Research & Therapy 11(3):229.
- Van den Berg WB. 2011. Osteoarthritis year 2010 in review: pathomechanisms. Osteoarthritis and Cartilage 19:338-341.
- Farnum CE, Wilsman NJ. 2011. Orientation of primary cilia of articular chondrocytes in three dimensional space. The Anatomical Record 294:533-549.