Edward Stevenson and Dr. Erin Bigler, Psychology and Neuroscience
Introduction
Autism is a developmental disorder. There has been an increasing trend in the diagnosis of autism in the past 15 years. After years of research there is still little agreement as to the causes of autism. It has been hypothesized that autistics could be the result of the body’s immune system attacking the brain through cytotoxicity and antibody mediated responses.2 Studies between immune factors and autism have had some interesting results, yet due to the complexities of the central nervous system and immune system, solid conclusions have not been reached.
My project investigated the presences of antibodies against two structural brain proteins, myelin basic protein (MBP) and glial fibrillary acidic protein (GFAP), in the blood serum of patients with autistic compared with healthy children. Autistic children were classified as classic or regressive onset autism, regressive implying that a child was developing normally and then developed autism whereas classic subjects with autism were apparently born with the disorder. The regressive distinction is suggestive of an environment trigger of the disorder such as mercury, virus, or psychological event.
Methods
All subjects were recruited by the Utah Autism Research Project (Salt Lake City), significant co-morbidities were excluded, and subjects were matched for age and gender. Blood was obtained, centrifuged, separated, and frozen. Immunoassay (western blotting) was performed and results scored. When antibodies are present a black band will appear at the location of the specific protein being investigated. A ubiquitous protein, histone 1 (H1), was used as a control. A control blot treated with mouse antibodies to MBP and GFAP was used as a positive control for each set of immunoassays performed. Immunoassay technicians were blind to all patient information. The order in which subjects were assayed was arbitrary with respect to grouping.
alysis and Results
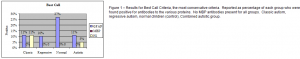
A variety of criteria was to determine positively scored blots to reduce bias in assessment. The Best Call criteria, the most conservative judgment, it reported here in Figure 1. The low occurrence of H1 is an indicator of the reliability of results for this criterion.
Autistic subjects were found to have less prevalence of antibodies than healthy controls in a roughly 3:1 manner for all judgment criteria. No distinction was observed between regressive and classic onset autism.
Discussion
From these results we conclude that antibodies to MBP and GFAP are not associated with autism. Preliminary data from Sweeten et al,3 using a different assay (ELISA) and the same patients and proteins has found autoantibody levels to MBP and GFAP lower than healthy controls but no statistical differences were found. My results are consistent with the results of the Sweeten et al study.
Studies from Singh’s4-6 laboratory have reported statistically higher numbers of autistic subjects compared with normal subjects with antibodies to MBP and GFAP. Their work has been highly cited yet no other laboratory has been able to reproduce their findings. My research does not confirm the work by Singh et al. Although smaller in size, my study was able to account for variables not previously accounted for in previous studies. Singh’s paper for MBP antibodies did not match for age. If only children-aged controls were analyzed in attempt to match for age, a chi-square analysis would result in a p=0.1176 which would fail to show statistically significant difference between normal and autistic subjects.
This study provides additional support for immune system irregularities in autism, but fails to contribute to an antibody mediated immune attack. Antibodies to other brain proteins may still be involved with autism. Further investigation in this area would be encouraged.
This study was published as an honor thesis. Data and literature research from this study will be included in a more extensive study to be published in the scientific literature in the near future. Research was also presented in poster formatted at various undergraduate research symposiums.
Figure 1 – Results for Best Call Criteria, the most conservative criteria. Reported as percentage of each group who were found positive for antibodies to the various proteins. No MBP antibodies present for all groups. Classic autism, regressive autism, normal children (control), Combined autistic group.
References
- Yazbak EF. Autism in the United States: A Perspective. Journal of American Association of Physicians and Surgeons. 2003 8(4):103-107.
- Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial Activation and Neuroinflammation in the Brain of Patients with Autism. Annals of Neurology. 2005 Feb; 57(1):67-81.
- Sweeten TL, Coon H, Burgess NK, McMahon WM, Fujinami RS. Antibody Studies in Autistic Disorder: Pathogens, Autoantibodies, Immunoglobulins? Unpublished Manuscript 2005. Correspondence to Robert.Fujinami@hsc.utah.edu
- Singh VK, Warren RP, Odell JD, Warren WL, Cole, P. Antibodies to Myelin Basic Protein in Children with Autistic Behavior- Brief communiciation. Brain, Behavior, and Immunity 1993; 7: 97-103.
- Singh VK, Warren RP, Averett R, Ghaziuddin M. Circulating Autoantibodies to Neuronal and Glial Filament Proteins in Autism-Brief Communication. Pediatric Neurology 1997; 17:88-90.
- Singh VK, Lin SX, Newell E, Nelson C. Abnormal Measles-Mumps-Rubella antibodies and CNS Autoimmunity in Children with Autism. Journal of Biomedical Science. 2002 Jul-Aug; 9(4): 359-364.