Kristina Hall and Dr. Wendy Birmingham, Psychology Department
Introduction
According to the Center for Disease Control and Prevention, about 79 million Americans are currently infected with HPV (“Human Papillomavirus (HPV)”, 2016). In fact, it is so common that most sexually active adults will be infected at some point in their life (“Human Papillomavirus (HPV)”, 2016). While HPV is in many cases innocuous, if it persists, certain strains may cause genital warts or several types of cancer. Nearly all cervical cancers are caused by HPV, along with many vulvar, vaginal, penile, anal, mouth and throat cancers (“HPV and Cancer”, 2016). Cervical cancer in particular is one of the most deadly cancers in American women, affecting about 12,990 women every year, and killing about 4,120 (“HPV and Cancer”, 2016). Fortunately, cervical cancer is preventable through HPV vaccination and regular Pap test screenings.
Despite the substantial benefits of HPV vaccination, many people still choose not to adhere to vaccination recommendations. Utah, a highly religious state, has HPV immunization rates far below the national average. As of 2015, only 24.6% of women in Utah are adherent to vaccination recommendations, compared to the national average of 41.9 % (Reagan-Steiner et al, 2016). The rates are even lower in men. Only 19.9% are completely adherent, compared to a national average of 28.1% (Reagan-Steiner et al, 2016). Other religious areas show similar patterns of HPV vaccine uptake (“HPV Vaccine Coverage Maps”, 2016) and negative attitudes toward the HPV vaccination (Shelton et al, 2013).
The reasons for the low vaccination adherence in religious areas of the western United States are not certain. In one study, parents cited reasons such as “don’t need vaccine”, “do not know enough about vaccine”, and “not sexually active” as rationale for not having their daughters vaccinated (Laz, Tahman & Berenson, 2012). In religious populations where abstinence and monogamy are key principles, people may be particularly prone to believing that their children are not at risk for contracting HPV and by extension cervical cancer because they teach their child to have one sexual partner who has also lived with perfect fidelity. However, many people fail to consider is that even an individual stays true to their values, they cannot control the behavior of their partner prior to or during marriage. Furthermore, circumstances such as divorce and remarriage or sexual assault unfortunately have the potential to expose an individual to HPV infection.
Parents and caregivers specifically play a key role in facilitating HPV vaccination. While the vaccine can still be administered up to age 26, the ideal time to vaccinate against HPV is early in the teenage years, a time when parents make most health decisions for their children and are primarily responsible for making medical appointments and staying up to date on vaccines. Therefore, this research was performed to examine knowledge, intentions, and attitudes toward the HPV vaccine of parents in highly religious communities in order to facilitate better understanding of the poor vaccination rates in Utah and other highly religious areas.
Methodology
The survey was created and distributed via Qualtrics. The survey includes basic demographic questions, relevant items from the literature to measure HPV and HPV vaccine knowledge, HPV and general vaccine attitudes, as well as health decision and healthcare information. Religiosity/spirituality was measured using the Religious Commitment Inventory-10 (Worthington et al., 2003). Participants were recruited through BYU SONA, flyers posted in the community, and social media. The survey was also distributed through colleagues in the Salt Lake County and San Diego County area. Participants were automatically screened for eligibility (i.e. whether not they currently had children between 11-18) by the survey system. After completing the survey, participants were offered the chance to enter a drawing for a $50 gift card. Quantitative frequency and regression data were analyzed using SPSS software version 25.
Results
The sample was majority female (91.6%), between 35-44 years old (53.1%), white (90.3%), with at least some college education (93.8%). Most of the sample was Latter-day Saint, though non-denominational Christian, Buddhist, Catholic, Jewish, Lutheran, and Methodist denominations were also represented. Quantitative analysis demonstrated that those with a more negative attitude toward the HPV vaccine were less likely to get the vaccine for their child (R=.406, p<.000) and those that scored lower knowledge about the HPV vaccine were less likely to vaccinate their children (R=.185, p<.031). More religious people also tended to have a more negative attitude toward the vaccine (R=.249, p<.000). Participants that indicated a higher level of religiosity were generally less likely to get the shot for their children (R=.223, p<.008).
Discussion
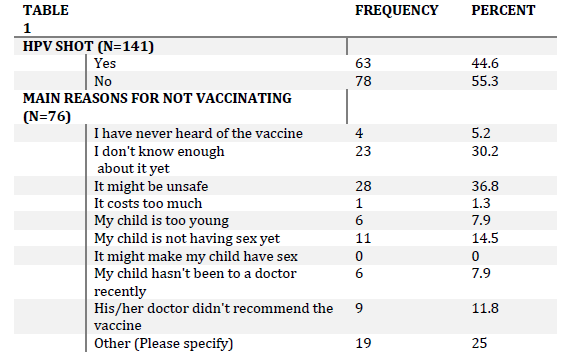
The results of the study indicate that negative attitude and lack of knowledge about the HPV vaccine is related to lower vaccine uptake, and that more religious people tend to both have a more negative attitude toward the vaccine and are less likely to have their children vaccinated. It is also important to understand some of the primary reasons participants indicated for not getting the vaccine. Rationale included not knowing enough about the vaccine, feeling that the vaccine is unsafe, or feeling that the vaccine is unnecessary/that their child is not at risk (Table 1). Strengths of the study include its diversity of sampling across religions and geographic locations. However, the study is somewhat limited in its small sample size at the time the analysis was done. Participants will continue to be recruited before the final analysis. Future studies could include focus groups or interviews to investigate the specificities of why people choose not to vaccinate, and perhaps investigate better ways to educate religious populations on the importance of the HPV vaccine.
Conclusion
Parents with higher levels of religious activity/spirituality are less likely to have their children vaccinated. Furthermore, this study demonstrated that they also tend to have a more negative attitude toward the vaccine and lack basic knowledge on HPV and the vaccine. Thus, when discussing the vaccine with patients, doctors or other educators should take their population into consideration. More religious parents may come in with a negative attitude toward the vaccine, without even really knowing what it is. With this in mind, it is important that discussions regarding the vaccine focus on educating parents on the importance, safety, and effectiveness of the HPV vaccine.