Jamie Cassinat and Renea Beckstrand, College of Nursing
Results
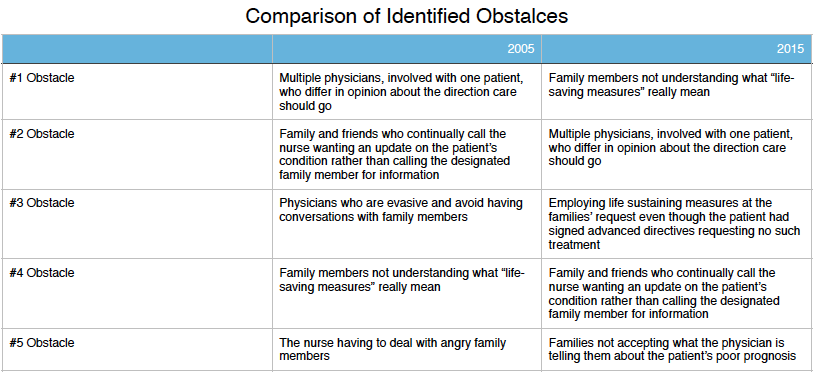
Identified Obstacles
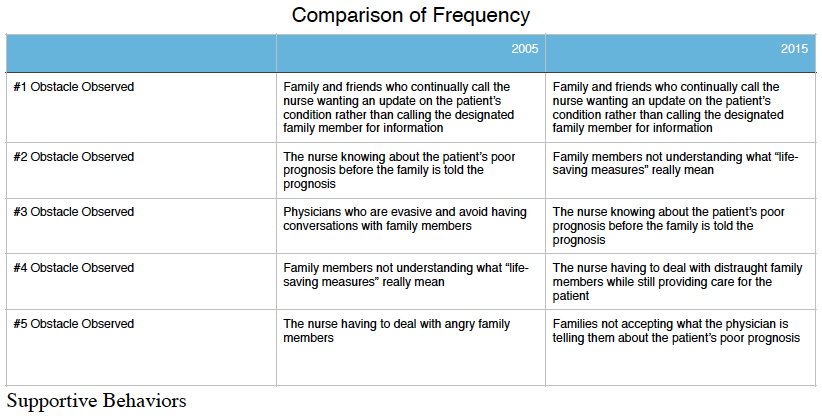
End of life care is an extremely sensitive time. Understanding variables, factors, and conditions that contribute to negative experiences makes it possible for interventions to be developed and implemented to ease an already stressful time. In addition to identifying obstacles, frequency of these obstacles occurring was also considered.
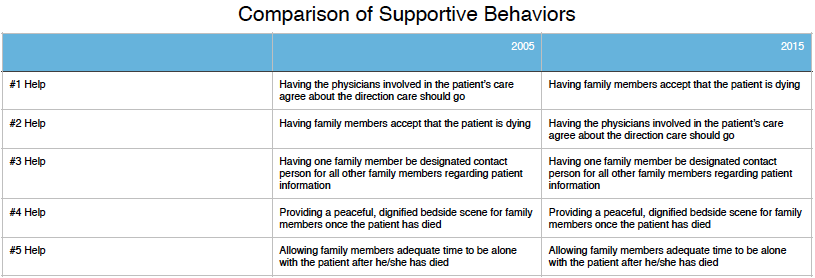
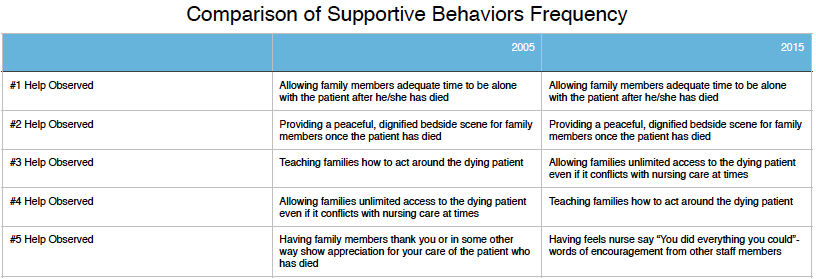
In addition to surveying nurses and asking what conditions impede ideal EOL care, participants were also asked to identify which practices were most helpful in easing EOL care and how frequently those practices were observed.
Recommendations
One barrier that was consistently noted was physicians not agreeing on patient prognosis and ideal plan of care. Facilitating communication amongst differing consulting physicians in a timely manner would ease EOL care. In addition educating family members regarding what “life saving measures” means and the implications of those decisions would also help EOL care.
One new emerging issue in the 2015 survey was that of accepting what the patient wished their treatment to be. Encouraging the general population and all newly admitted patients to write advance directives would help with this barrier. In addition a new emerging supportive behavior identified in the 2015 survey was helping not only physicians but family members to agree on treatment for their loved ones.
Supportive behavior that should be continued include: having one contact person in the family as an information source, in addition allowing for enough time to have a peaceful bedside scene was consistently viewed as helpful in EOL care.