Zachary McDonnell and Dr. Erin Bigler, Psychology Department
Introduction
The Cache County Study on Memory in Aging (CCMA) includes a sample of over 400 individuals with magnetic resonance imaging (MRI) (Bigler et al., 2000). Studies have shown that White Matter Hyperintensities (WMH) on MRIs are associated with not only cognitive decline, but degenerative disorders like Alzheimer’s disease (Philip Scheltens et al., 1998). A common and widely used clinical rating method for identifying WMH is the Scheltens Rating Scale (PH Scheltens et al., 1993). This scale rates WMH, Grey Matter Hyperintensities (GMH), Periventricular White Matter Hyperintensities (PWM), and Infratentorial Signal Hyperintensites (IFH) in a semi-quantitative scale that can be easily taught to raters with little to no background in neuroimaging and is as reliable as other more complex or automated scales. Our goal in this research was to investigate severity WMH and determine its predictive effect on cognitive scores and life expectancy.
Methodology
Overall in the CCMA approximately 80% of the individuals were between 80 to 95 years of age and 99% were Caucasion. Among the 415 subjects, 51% had some high school or below high school education, 34% had some college education, and 14% had higher than college education. To measure cognitive ability the Mini-mental state exam (MMSE) was used. This exam is short and the questions are designed to analyze several domains of cognitive function.
MRI scans were derived from a .5 Tesla MRI machine. This machine took axial proton density images along with T2-weighted images. A coronal cut of the T2-weighted images was also obtained. Scan thickness was 5.0 mm with slice spacing of 2.0 mm and in each image set there were approximately 40 slides. The T2-weighted images were used to assess WMH, while the proton density images served as a reference point for identification.
The raters were undergraduates at BYU, trained to use the Scheltens rating system and they used both the axial and coronal planes to assess WMH. Initially, raters underwent a month of intensive training by Dr. Bigler followed by weekly training throughout the study. Data was periodically analyzed to assess their inter-rater reliability. Each scan received two ratings and if a scan received significantly different ratings, Dr. Bigler gave the final rating.
Results
Cronbach alpha was used to determine the inter-rater reliability. Cronbach alpha is scale from 0- 1 and consistent data should have a .85 or above. Our raters had a Cronbach alpha of 0.891. The Schelten Scale has an overall scale from 0-96 and our standard deviation decreased from 9 scale points during training down to 3.63 overall—this was calculated before Dr. Bigler’s review.
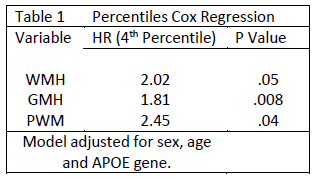
Overall, MMSE negatively and significantly related to WMH (r=-0.22, p<0.05), GMH (r=-0.15, p<0.05), PWM (r=-0.23, p<0.05), and Scheltens total score (r=-0.24, p<0.05). No significant relationship was found between MMSE and IFH (r=-0.06, p<0.05). We ran two Cox regressions on the data, one to determine MCI conversion to dementia and the other for conversion from life to death. Both were calculated by taking the number of days from the MRI scan to the diagnosis of dementia or death. No significant results were found for MCI conversion to dementia. In the second Cox regression both GMH and PWM were robust in predicting time till death (See Table 1). PWM was particularly robust and remained significant in various models of the Cox regression not presented here.
Discussion
 We were extremely satisfied with the consistency of the data produced by undergraduates. Originally we didn’t know how well we could train students to rate radiological data but inter-rater reliability scores were very promising and for the last set of 220 scans only 7.9% needed to be reviewed by Dr. Bigler.
We were extremely satisfied with the consistency of the data produced by undergraduates. Originally we didn’t know how well we could train students to rate radiological data but inter-rater reliability scores were very promising and for the last set of 220 scans only 7.9% needed to be reviewed by Dr. Bigler.
As expected, MMSE was negatively correlated with WMH which holds to the idea that hyperintensities are indicative of deterioration of the brain. It was disappointing that WMH were not predictive of MCI conversion however our result wasn’t unusual. WMH are indicative of vascular decay and dementia is a broad category that includes all types of dementia besides vascular dementia. Even after analyzing data for only vascular dementia there wasn’t enough scans to reach statistical power for significant results.
We were surprised to find the robustness of PWM over all other hyperintensities in the brain but again this result is logical. If hyperintensities are an indicator of vascular decay then vascular decay will most often occur at the peripheral edge of the vascular system in the brain. Many of the capillaries for the brain end in the PWM.
Conclusion
Overall it was encouraging to find that significant results could be obtained through undergraduates and that WMH overall correlates with life expectancy. Even using a general scale like the Schelten Scale we calculated a significant hazard ratio of 2.02 for PWM. More research is needed to determine exactly where in the PWM that contributes to life expectancy and MCI conversion. With a clearer understanding of WMH and the regions of the brain that contribute to MCI conversion, this significant results could lead to better predictive measures for those with Dementia.
Bibliography
Bigler, E. D., Lowry, C. M., Anderson, C. V., Johnson, S. C., Terry, J. & Steed, M. (2000). Dementia, quantitative neuroimaging, and apolipoprotein E genotype. American journal of neuroradiology, 21(10), 1857–1868. Am Soc Neuroradiology.
Scheltens, Philip, Erkinjunti, T., Leys, D., Wahlund, L.-O., Inzitari, D., del Ser, T., Pasquier, F., et al. (1998). White matter changes on CT and MRI: an overview of visual rating scales. European neurology, 39(2), 80–89. Karger Publishers.
Scheltens, PH, Barkhof, F., Leys, D., Pruvo, J., Nauta, J., Vermersch, P., Steinling, M., et al. (1993). A semiquantative rating scale for the assessment of signal hyperintensities on magnetic resonance imaging. Journal of the neurological sciences, 114(1), 7–12. Elsevier.
