Mary Kent and Dr. Catherine Burnham, School of Family Life
Antimicrobial textiles are on the cutting edge of fiber nanotechnology and are a new concept in the textile industry. Antimicrobial textiles are fabrics covered in a unique silver finish that helps to prevent infection. Research has repeatedly shown their effectiveness to prohibit growth of microorganisms, such as bacteria, fungi, and algae. This particular effect makes them applicable and very useful in the healthcare industry, and several different products such as dressings, masks, and gowns have been developed for healthcare use. Despite their shown effectiveness, before I started my own research, there was a dearth of information showing whether health care professionals were aware of these products.
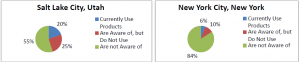
The goal of my investigation was to compare and study two different direct marketing areas (DMA’s) in regards to antimicrobial textiles being used by medical professionals. This project was focused first on whether medical professionals are aware of antimicrobial textiles; secondly, if there are advantages that large cities have over smaller cities in incorporating technological advances into healthcare practice because of the greater quantity of research preformed within. In order to do this, I conducted multimethod interviews with medical professional to discuss their awareness and use of antimicrobial textiles within their own practice. I surveyed 102 medical professionals. The individuals were divided up evenly into two DMA’s: 51 from Salt Lake City, Utah, and 51 from New York City, New York.
My main task was to gather information. I formulated three separate and short surveys that varied according to the awareness of the medical professional. I contacted them using web, phone, and face-toface interactions. When I surveyed them, the first question I asked the individual was: “Do you currently use antimicrobial products, have you heard of them, or have you not heard of them?” Their answer out of the three options indicated the correct survey to complete. Questions that followed helped me understand the depth of their knowledge and frequency in use of the products.
My original hypothesis was that due to the fact that New York City is the largest city in the United States, and because it is a leader in the textile and healthcare industries that the medical professionals would be more informed and familiar with antimicrobial textiles than those professionals in Salt Lake City. As one can see in the graph provided below to show my quantitative findings, the results were very surprising for me, and my hypothesis was shown as incorrect. The graph shows a lack of awareness of antimicrobial textiles, not only in both cities, but especially in New York City. It also shows that Utah had a higher percentage of professionals that were more aware of the textiles.
Looking at the quantitative findings, there could be a number of factors that may have influenced the data. First, my N size was somewhat small to accommodate my being a student as well. In order to get a more complete picture of medical professionals’ awareness of these products, it would be effective to increase the N size in each DMA to get a larger picture.
Another factor could be a matter of who was available to speak with me. Although I spoke with many doctors, who are usually the ones who mandate what materials are used in their practice, I also spoke with many nurses. Even individuals in the same office had different levels of familiarity with the products. For example, I interviewed a nurse who had not even heard of them, and after I spoke with the nursing manager from the same unit. He actually took me around the hospital areas and showed me the antimicrobial products that they were currently using. As mentioned earlier, a larger N size might be able to more truly depict the knowledge of professionals in each DMA.
After my first question (quantitative), I asked more qualitative questions to understand the individual’s responses. For those that currently used it, I asked the professionals to rate them on a scale of one to ten according to effectiveness in infection reduction, healing time, and odor reduction. The answers were frequently a nine or a ten. Cost of the products was only one category in which they received lower ratings, such as fours or fives, as they are very expensive products. Many of them also expressed that they use the products daily or weekly. Every burn unit in each city used antimicrobial dressings, as they do not have to be changed as often as traditional dressings (which help patient comfort), and help reduce infection.
For those professionals who had heard of antimicrobial products, I found that there were two major reasons that they were not using them, and it seemed to depend on their understanding of what they were. Some professionals became aware of them (either through a colleague or conference) but were not convinced that they were worth the high cost for a ‘small’ return rate, and also that traditional hand washing and sanitation practices should suffice. Other professionals were aware of them from conferences, magazine reports, or advertisements and expressed the desire to research them further for a better understanding of the product possibilities. As for the professionals who had never heard of antimicrobial products, before questioning, I read a short paragraph explaining what they were. A majority of those interviewed agreed that they would probably be useful due to the fact that they reduce infection, but they also noted a need for personal research in order to feel justified in using the products.
As I researched professionals’ awareness of the textiles, I also became more educated about different antimicrobial products other than just masks, gowns and dressings. I also found that some hospitals use antimicrobial fabric curtains. In the realm of other textiles, there are antimicrobial catheters and thermometer heads that are currently being used. Overall, the most popular use of all antimicrobial products in my research is the wound dressings.
The opportunity to take matters into my own hands and find data on something that fascinates me was a great learning experience. I have written a newspaper article about antimicrobial products and my findings and have recently submitted it to Textile World, Zirmed, and The Family and Consumer Science Research Journal, and I am hopeful it will be published. I also have contacted the College of Nursing at BYU to set up an in-service in order to raise awareness to contribute to the solution of more needed knowledge of antimicrobial textiles.
