Luke Reed Wilding and Dr. Alonzo Cook, Chemical Engineering
Introduction
Whenever someone has a serious traumatic injury and has damage to the peripheral nerves it is very common to lose motor function in that area of the body due to slow axon regeneration. For example, if someone were to severely cut their arm above the elbow they would lose motor and sensory functions in the distal parts of their arm unless there were some types of effective treatment. Currently, the main treatment is to take a nerve from the ankle area of the person (an autograft) in order to fill the gap in the severed nerve. While this process does work well, the patient sacrifices feeling and response from the nerves in their foot. In Dr. Cook’s lab we have the goal to replace the autograft with a nerve allograft that won’t have an immunogenic response upon implantation. Our method was to remove all the immunogenic cells from rat sciatic nerves through a process called decellularization, culture Schwann cells through the nerve to create the nerve graft, and then implant the nerve into the rat.
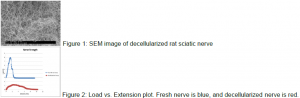
My project took a smaller part of the overall project that has been conducted in Dr. Cook’s lab. I worked on different methods to quantify the integrity of the nerve matrix before and after we removed the immunogenic cells through decellularization. However, we were concerned that our process would degrade the collagen network that provided the structure to the nerve. We used a harsh chemical solution consisting of a small concentration of sodium dodecyl sulfate (SDS), that would break cell membranes and remove all of the cells that identify a nerve, leaving the collagen behind. The collagen looks like a large web network (Figure 1). The collagen network provides scaffolding for the neurons to pass through. The scaffolding provides the strength, stability, and environment for neurons to survive.
Methodology
In order to quantify the integrity of the collagen matrix, I conducted two main tests, one that was qualitative and one that was quantitative. The quantitative test was to visually inspect our decellularized nerves using a scanning electron microscope at the microscope lab here at BYU. We prepared the nerves and were able to obtain many images that gave us a good idea of the integrity of the collagen matrix (Figure 1).
The second test that I conducted required the use of another lab here at BYU. We were able to use an Instron machine in the Mechanical Engineering lab to measure the tensile strength of three groups of nerves. The three groups were fresh nerves, crushed nerves, and decellularized nerves. An Instron machine pulls a specimen on both ends until the specimen breaks. These machines are traditionally used to measure tensile strengths of metals or plastics, but we used special fixtures that could clamp down on the nerves and pull them until failure. We were then able to measure the force required to break the nerve, which gave us a good measurement of the overall strength and integrity of the nerve matrix (Figure 2).
Results
Through tensile testing we were able to compare the strength of fresh nerves with 2 other groups of nerves; a decellularized group and a crushed nerve group. Based on our analysis of the stress vs. strain curves, the fresh nerves had the greatest tensile strength. They were able to withstand a load of around 8 Newton’s on average, while the decellularized group only withstood a load of about 2 Newton’s on average (see Figure 2).
Through our analysis of the decellularized nerve matrix, we were able to see that we removed all of the cells excluding the collagen. The collagen itself appeared to be intact, but there was very little of other types of tissue that could act to help the structural integrity as well.
Discussion
Based on the results we were able to obtain, we did see a significant decrease in strength based on our decellularization process. This significant decrease could be due to many different factors, but by removing all of the immunogenic cells, we are removing some of the structural filler of the cells. This may be similar to removing cement from rebar scaffolding, which would significantly reduce the strength of a structure.
There was also a significant variation based on the size of each rat that we used. Some nerves were longer and thicker than others. Also, there was a significant variation on the method of nerve extraction. Depending on the student who performed the dissection and nerve extraction there could be differences in the cuts that were made as well as the locations of the cuts.
We also saw some variation in the nerve strength testing. We used metal adaptors with sandpaper lined clamps that pinched on the ends of the nerve. In some of the tests we saw some slipping that affected the overall tensile strength data.
Conclusion
Based on the results that we were able to obtain, our decellularized nerves showed a significant reduction in strength. However, we are still in the process of testing the ability of these nerves to assist in nerve regeneration. It may be that even with reduced structural strength, having a nerve implant without immunogenic properties can help create a favorable environment for nerve regeneration.