Jonathan Jacobs, Katreena Collette-Merrill RN PhD, College of Nursing
Introduction
The culture of education prepares healthcare professionals in silos, then expects them to work collaboratively upon graduation. Medical errors, resulting from communication issues, are considered a leading cause of patient death. Interdisciplinary education of future professionals may prevent communication issues and reduce patient deaths. Interprofessional education (IPE) of undergraduates may improve communication of future professionals educated in universities without medical schools. The purpose of this project is to evaluate the effect of interprofessional education (IPE) on undergraduate students’ attitudes of interprofessional work, perceptions of working together, and ratings of teamwork.
Research Questions: Following a semester-long IPE class:
1. What are students’ attitudes toward IPE and opinion of usefulness of IPE activities?
2. How do students describe their perceptions about ability to, value of, and comfort in working in interprofessional teams?
3. What are students’ ratings of teamwork, interprofessional interactions, and relationships?
Methodology
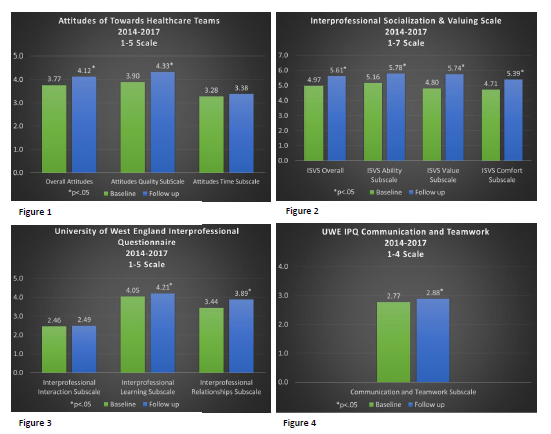
Methodology: A pre-post descriptive quantitative design was used. A total of 127 undergraduate students enrolled and completed questionnaires at the beginning and end of the Interprofessional Education for the Health Professions course. Study subjects included students of the following majors: nursing, dietetics, medical lab science, public health, exercise science, and pre-professional (pre-medical, pre-dental, etc.). Quantitative data included survey results of three validated instruments used in IPE research including: Attitudes Towards Healthcare Teams (ATHCT), with two subscales; Interprofessional Socialization & Valuing Scale (ISVS), with three subscales; and The University of West England Interprofessional Questionnaire (UWE IPQ), with 4 subscales. Data were analyzed using a two-tailed paired t-test.
Results
Student responses showed significant increases in IPE scores on all except for two of the subscales. Students participating in the interprofessional course reported significantly increased overall scores on the ATHCT and the Quality of Care subscale (p = .000; 5-point Likert-type; see figure 1). Students also reported significantly increased overall ISVS scores and on all 3 subscales (p = .000; 7-point Likert-type; see figure 2). Students reported significantly increased scores on the Interprofessional Learning, Relationships, and Communication and Teamwork subscales of the UWE IPQ (p < .015; 5-point Likert and 4-point Likert-types; see figures 3 and 4).
Discussion
Students’ perceptions of interprofessional collaboration improved on most, but not all the subscales of the instruments used; therefore, IPE may be useful to augment health education of undergraduates when used in conjunction with hospital experiences. One limitation of this research is the high response burden (there were 73 items in the questionnaire), and another limitation is that perceptions of graduates in the workforce were not measured. Future research may improve completed response rates through shorter questionnaires and may also elucidate long-term effects of IPE.
Conclusion
IPE of undergraduate students in health-related majors can significantly improve their attitudes toward interprofessional collaboration according several validated instruments. IPE may not completely substitute for real hospital interaction, but may be used in conjunction with hospital experiences to improve the interprofessional collaboration of