Jonathan Jacobs and Faculty Mentor: Katreena Collette-Merrill RN PhD, Nursing
Introduction
The culture of education prepares healthcare professionals in silos, then expects them to work collaboratively upon graduation. Medical errors, resulting from communication issues, are considered a leading cause of patient death. Interdisciplinary education of future professionals may prevent communication issues and reduce patient deaths. Interprofessional education (IPE) of undergraduates may improve communication of future professionals educated in universities without medical schools. The purpose of this project is to evaluate the effect of interprofessional education (IPE) on undergraduate students’ attitudes of interprofessional work, perceptions of working together, and ratings of teamwork.
Research Questions: Following a semester-long IPE class:
1. What are students’ attitudes toward IPE and opinion of usefulness of IPE activities?
2. How do students describe their perceptions about ability to, value of, and comfort in working in interprofessional teams?
3. What are students’ ratings of teamwork, interprofessional interactions, and relationships?
Methodology
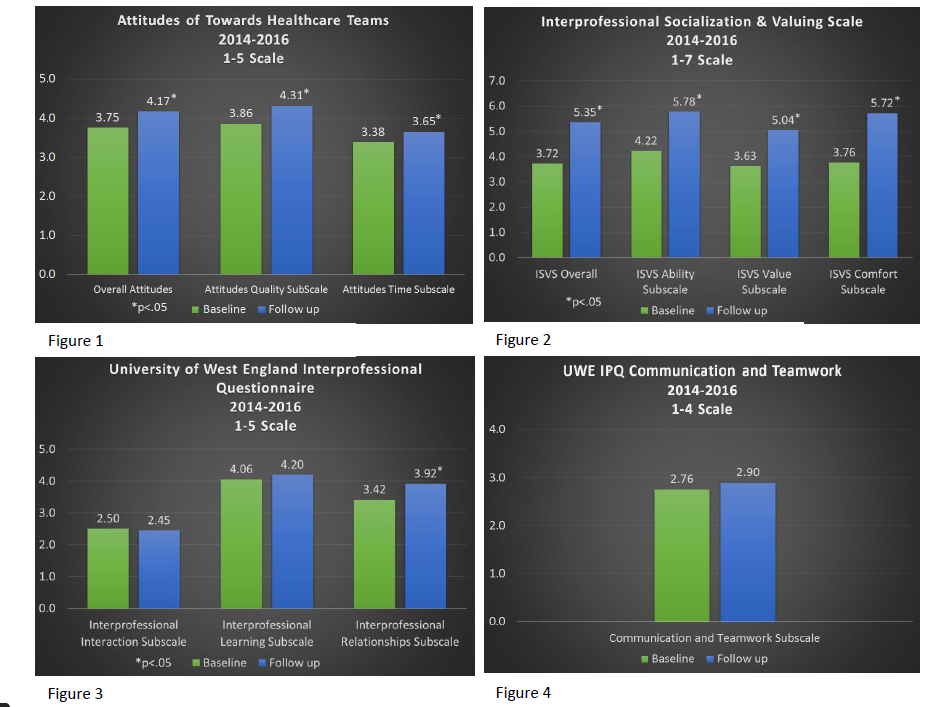
Methodology: A pre-post descriptive quantitative design was used. A total of 110 undergraduate students enrolled and completed questionnaires at the beginning and end of the Interprofessional Education for the Health Professions course. Study subjects included students of the following majors: nursing, dietetics, medical lab science, pre-professional, public health, exercise science, and other health-related professions. Quantitative data included survey results of three validated instruments used in IPE research including: Attitudes Towards Healthcare Teams (ATHCT), with two subscales; Interprofessional Socialization & Valuing Scale (ISVS), with three subscales; and The University of West England Interprofessional Questionnaire (UWE IPQ), with 4 subscales. Data were analyzed using a two-tailed paired t-test.
Results
Student responses showed significant increases in IPE scores with two of the three instruments. Students participating in the interprofessional course reported significantly increased overall scores on the ATHCT and on both subscales (p = .000; 5-point Likert-type; see figure 1). Students also reported significantly increased overall ISVS scores and on all 3 subscales (p = .000; 7-point Likert-type; see figure 2). The results of the UWE IPQ (5-point Likert and 4-point Likert-types; see figures 3 and 4) were mixed. Students reported significantly increased scores on the interprofessional relationships subscale (p = .000; 5-point Likert-type). Students’ scores on the other three UWE IPQ subscales were not significant.
Discussion
Student perceptions did not significantly change on three of the UWE IPQ subscales; therefore, IPE of undergraduates may not be a complete substitute for hospital interaction IPE of future health professionals in the undergraduate setting. However, since IPE can significantly improve students’ perceptions toward interprofessional collaboration according to several validated instruments, IPE may be useful to augment health education of undergraduates when used in conjunction with hospital experiences. One limitation of this research is the sample size; with a larger sample size we may find significant changes on more subscales of the UWE IPQ, and be able to look for possible variations in scores according to major of undergraduate students.
Conclusion
IPE of undergraduate students in health-related majors can significantly improve their attitudes toward interprofessional collaboration according several validated instruments. IPE may not completely substitute for real hospital interaction, but may serve as a good augmentation toward interprofessional collaboration of future health professionals, which should be used in conjunction with experiences in hospital settings.